Hypocalcemic tetany is an uncommon condition in horses caused by exertion, transport, or lactation. Signs vary in type and severity. Diagnosis is based on signs, serum calcium levels, and response to treatment. Slow intravenous administration of calcium usually leads to full recovery. Reducing stress and fasting during transport can help prevent the disorder. Pregnant mares should be fed adequate amounts and ratios of calcium and phosphorus throughout pregnancy to prevent lactation tetany.
Hypocalcemic tetany in horses is an uncommon condition associated with acute depletion of serum-ionized calcium and sometimes with alterations in serum concentrations of magnesium and phosphate. It occurs after prolonged physical exertion or transport (transport tetany) and in lactating mares (lactation tetany). Signs are variable and relate to neuromuscular hyperirritability. Hypocalcemia also causes decreased intestinal motility, so colic signs are also present.
Etiology of Hypocalcemic Tetany in Horses
Mechanisms of hypocalcemia include decreased absorption from the intestines; increased loss of calcium from the kidneys, sweat, or milk; or inhibition of osteolysis due to alterations in parathyroid hormone, calcitonin, or vitamin D. In lactating mares, high milk production and grazing of lush pastures appear to be predisposing factors. Hypocalcemia after prolonged physical activity (eg, endurance rides) results from sweat loss of calcium, increased calcium binding during hypochloremic alkalosis, and stress-induced high corticosteroid levels. Corticosteroids inhibit vitamin D activity, which leads to decreased intestinal absorption and skeletal mobilization of calcium. Stress and lack of calcium intake have been associated with transport tetany. Occasionally, hypocalcemic tetany may be precipitated by hypocalcemia after blister beetle ingestion. Administration of bisphosphonates may also cause hypocalcemia shortly after the drugs are administered.
Clinical Findings of Hypocalcemic Tetany in Horses
The severity of clinical signs corresponds with the serum concentration of ionized calcium. Increased excitability may be the only sign in mild cases.
Severely affected horses may show:
anxious appearance
signs of tetany, including:
increased muscle tone
stiffness of gait
muscle tremors
prolapse of the third eyelid
inability to chew
trismus
salivation
recumbency
convulsions
cardiac arrhythmias
In lactating mares, if not treated, the disease may take a progressive and sometimes fatal course over 24–48 hours.
Diagnosis of Hypocalcemic Tetany in Horses
Confirmation of low serum levels of ionized calcium or possibly total serum calcium
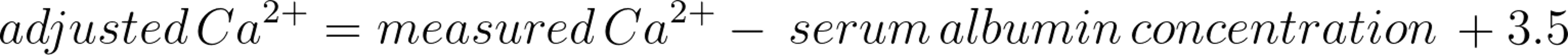
A tentative diagnosis is based on clinical signs, history, and response to treatment. Definitive diagnosis requires demonstration of low serum levels of ionized calcium. Most laboratories measure only total (protein-bound and free) serum calcium, which is an acceptable diagnostic test in most cases. However, discrepancies may arise in alkalotic and hypoalbuminemic horses. Alkalosis increases albumin binding of calcium, which results in a decreased concentration of ionized calcium. Thus, alkalotic horses may have normal total serum calcium while exhibiting signs of hypocalcemia. Likewise, hypoalbuminemic or acidotic horses may have decreased total serum calcium without developing signs of hypocalcemia. Total serum calcium can be adjusted for albumin concentration by the following formula:
Differential diagnoses include:
endotoxemia
exertional rhabdomyolysis or other muscle disorder
seizure disorder
Treatment of Hypocalcemic Tetany in Horses
IV of calcium solutions
In treating hypocalcemic tetany in horses, intravenous administration of calcium solutions, such as 20% calcium borogluconate or solutions recommended for treatment of periparturient paresis in cattle, usually results in full recovery. These solutions should be administered slowly (throughout 20 minutes) at 250–500 mL/500 kg, diluted at least 1:4 in saline or dextrose, and the cardiovascular response should be closely monitored. An increased intensity of heart sounds is expected. If arrhythmias or bradycardia develop, the IV treatment should be discontinued immediately. Once the heart rate has returned to normal, the infusion may be resumed at a slower rate. If the horse does not improve within 1–2 hours of the initial infusion, a second dose may be given, although laboratory verification of hypocalcemia is indicated.
Some horses require repeated treatments throughout several days to recover from hypocalcemic tetany. Mildly affected horses may recover without specific treatment. If the tetany is associated with physical exertion, incorporating magnesium into the solution may be advisable.
Prevention of Hypocalcemic Tetany in Horses
A balanced feed ration should be provided to supply adequate amounts and ratios of calcium and phosphorus throughout gestation. In times of increased calcium demand such as lactation, fasting should be avoided, and high-quality forage such as alfalfa or calcium-containing mineral mixes should be provided. Stress and fasting during transport should be minimized. In endurance horses, water and electrolyte deficits associated with prolonged exercise and sweating may be prevented by provision of a sufficient water supply and electrolyte supplementation.
Bisphosphonate use should be avoided or used with caution in horses with conditions affecting mineral or electrolyte homeostasis (for example, hyperkalemic periodic paralysis or hypocalcemia) or conditions that may be worsened by hypocalcemia (for example, cardiac disease). Bisphosphonates are contraindicated in horses with renal disease.
Key Points
Clinical signs of hypocalcemia include colic, synchronous diaphragmatic flutter, or tetany.
Diagnosis is based upon clinical signs and low serum ionized calcium concentrations.
Intravenous calcium and provision of alfalfa (lucerne) hay typically result in rapid resolution of clinical signs.